In the healthcare sector, Medicare, and credentialing play crucial roles in ensuring high-quality care and patient safety. Millions of Americans have access to Medicare’s health coverage, which enables medical professionals to deliver necessary services to eligible beneficiaries. For instance, Medicare enables medical professionals to deliver essential services to the elderly, while credentialing provides patients with the assurance that their healthcare providers have attained high levels of professionalism and competence.
Understanding Medicare
Americans over the age of 65 are normally covered by Medicare, a government-run health insurance program. Additionally, it helps some younger individuals with impairments or end-stage renal illness.
It’s important because it ensures that millions of Americans will have access to reasonably priced healthcare.
Medicare consists of different parts that offer coverage for specific healthcare services:
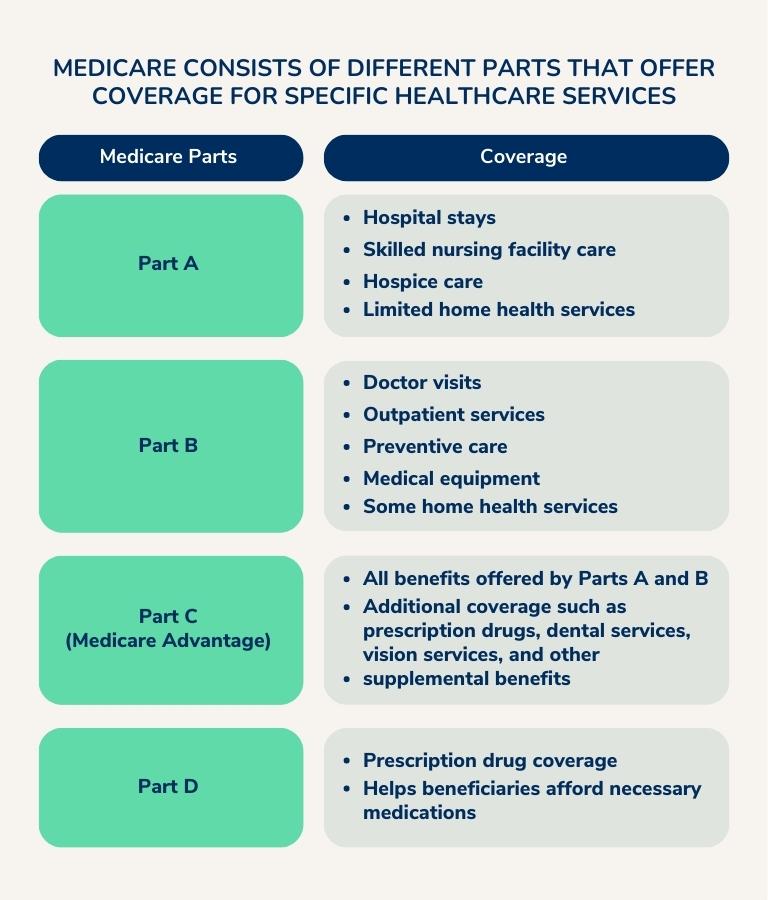
Some key aspects to keep in mind are:
- Age and/or disability status are the main factors that determine eligibility for Medicare.
- Typically, the registration period starts three months before a person turns 65 or during a specified Special registration Period.
- The Social Security Administration offers comprehensive instructions and information on the Medicare enrollment and eligibility process.
- Many individuals hold false assumptions about Medicare, such as that it is equivalent to Medicaid or that it covers all medical expenses.
- The official website for Medicare, medicare.gov, offers resources to clear up common misconceptions and provide accurate information about Medicare as well as a complete list of frequently asked questions.
To understand more one can, glance over “Medicare Advantage 2020 Spotlight: First Look,” research by the Henry J. Kaiser Family Foundation, which offers an in-depth review of the patterns and data surrounding Medicare Advantage plans and provides insights into the benefits and rising popularity of Part C coverage alternatives.
There are several Medicare applications that healthcare providers may need to fill out depending on their specific circumstances. Here are a few examples:
- CMS-855A: This is used for initial enrollment and revalidation of Medicare enrollment for institutional providers, such as hospitals and skilled nursing facilities.
- CMS-855B: This application is used for initial enrollment and revalidation of Medicare enrollment for group practices and other non-institutional providers.
- CMS-855I: This application is used for initial enrollment and revalidation of Medicare enrollment for individual practitioners, such as physicians, nurse practitioners, and physician assistants.
- CMS-855O: This application is used for ordering and certifying eligibility for Medicare home health services.
- CMS-855S: This application is used for initial enrollment and revalidation of Medicare enrollment for suppliers of durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS).
- 855R: This application is used to reassign Medicare benefits from one provider to another.
Navigating the Credentialing Process
Our goal is to streamline and expedite the provider application process for various healthcare networks, including Medicare, Medicaid, Aetna, Cigna, UnitedHealthcare, TRICARE, and many others. Here’s how we can help you complete your applications twice as fast:
- Streamlined Application Filing: We provide a comprehensive checklist and handle the filing of contract applications, ensuring flawless submissions and shorter turnaround times.
- Effective Network Research: Our experienced team conducts thorough research to help you build a diverse and effective mix of popular payors. We provide accurate enrollment timelines for Medicaid, Medicare, and commercial payers.
- Out-of-Network Enrollments: If you choose to stay out of network or face closed panel situations, we guide you through the enrollment process to ensure your practice is registered in Medicare’s system for seamless payments.
- Simplified EFT and ERA Enrollments: We assist in setting up Electronic Funds Transfer (EFT) and Electronic Remittance Advice (ERA) enrollments, streamlining your financial transactions.
- Efficient Demographic Updates: We handle all changes to your demographics, such as updates to your bank account, address, or TAX ID, ensuring accurate and up-to-date information.
- Expert Contract Negotiations: Our team negotiates contracts and fee rates on your behalf, utilizing our extensive database of the latest fee schedules to obtain the best possible rates.
- CAQH and PECOS Compliance: We maintain and update your CAQH and PECOS profiles, ensuring compliance and accuracy with these important credentialing systems.
- Thorough Application Follow-Up: Our enrollment team regularly follows up on your applications, confirming receipt and monitoring for any additional information requests from Medicare.
- Appeals for Closed Panels: We handle appeals for closed panel situations, submitting comprehensive business plans to Medicare’s senior provider representatives to increase the chances of overturning decisions.
- Comprehensive Credentialing Maintenance: Our credentialing portal provides transparent and HIPAA-compliant management of your providers’ credentials, ensuring accurate data for larger healthcare facilities.
- Dedicated Support: Our specialists provide personalized support throughout the credentialing process.

Enrollment Process with Medicare
To become credentialed with Medicare as a new provider, here are the general steps we follow to assist you better:
- Obtain an NPI: Apply for a National Provider Identifier (NPI) online or by mail.
- Secure Malpractice Coverage: Purchase medical malpractice insurance and keep a copy of the declaration page.
- Access PECOS: Use the Medicare enrollment system, PECOS, to begin the process.
- Gather Documentation: Collect required documents like your NPI number, state license, resume, and malpractice insurance details.
- Complete Enrollment Application: Fill out the Medicare provider enrollment application through PECOS.
- Seek Assistance: Contact Medicare phone support for help during the application process.
- Collaborate with MAC: Work with your Medicare Administration Contractor (MAC) and provide any additional requested information.
- Choose Specialty Designation: If applicable, select a specialty designation that aligns with your profession.
- Pay Application Fee: Submit the necessary application fee for initial enrollment or revalidation.
Application Process to Become a Provider
- Ensure Proper Date on the Signature Page – Ensure Proper Date on the Signature Page
- Complete Demographic Information Correctly – Fill in all requested demographic details in Section 2 accurately.
- Use IRS-Approved Business Name – Enter your business name exactly as shown on IRS documents and CP-575.
- Include Valid Bank Account Verification – Include a voided check or bank account verification letter with the correct company name.
- Provide Direct Contact Details – Use your contact information for direct communication, avoiding third-party involvement.
- Sign the Form in Blue Ink – Use blue ink to sign the form, preventing any confusion or rejection.
Challenges and Strategies for Overcoming Common Obstacles and Ensuring Compliance

Benefits for Healthcare Providers with Apaana
- Expanded Patient Base: Participating in Medicare allows healthcare providers to access a large pool of potential patients, including the elderly and individuals with disabilities who qualify for Medicare coverage.
- Reliable Reimbursement: Medicare offers a predictable and reliable reimbursement system, reducing financial uncertainty for providers compared to private insurance plans.
- Enhanced Reputation and Trust: Credentialing validates healthcare professionals’ qualifications, fostering trust and confidence among patients, healthcare organizations, and insurance networks.
- Streamlined Administrative Processes: Credentialing facilitates streamlined communication and coordination with healthcare facilities, insurers, and regulatory bodies, simplifying administrative tasks.
- Access to Resources and Support: Medicare provides access to resources, educational programs, and quality improvement initiatives that can enhance clinical practices and patient outcomes.
In conclusion, understanding Medicare and navigating the credentialing process are crucial for healthcare providers. Apaana Healthcare, a credentialing outsourcing agency, offers solutions to expedite the application process for Medicare and other providers. Their streamlined filing, effective research, simplified enrollment, and comprehensive maintenance services can help providers complete applications twice as fast. By partnering with Apaana Healthcare, healthcare professionals can ensure compliance, enhance their reputation, and expand their patient base. Contact Apaana Healthcare today to accelerate your Medicare enrollment and credentialing process.
References
- Medicare.gov – The official website for Medicare, providing accurate information and resources about Medicare coverage, eligibility, and frequently asked questions. Link: Medicare.gov
- Henry J. Kaiser Family Foundation – Research organization that offers in-depth studies and insights into Medicare Advantage plans, including an analysis of trends and data. Link: Medicare Advantage 2023 Spotlight: First Look | KFF
- Centers for Medicare & Medicaid Services (CMS) – The federal agency that administers the Medicare program, providing applications and enrollment information for healthcare providers. Link: Become a Medicare Provider or Supplier | CMS
- CAQH – A nonprofit alliance that offers credentialing and provider data management services, including maintaining and updating CAQH profiles. Link: CAQH
- PECOS – The Medicare Provider Enrollment, Chain, and Ownership System, where healthcare providers can begin the enrollment process with Medicare. Link: PECOS